Single cell and AI team up to find biomarkers for targeted therapy response in chronic myeloid leukemia
Artificial intelligence continues to infiltrate our lives. For example, recently, scientists combined single cell experiments with machine learning algorithms to create a transcriptional map of treatment resistance in patients with chronic myeloid leukemia (CML). They identified eight overarching factors that determine drug response as well as two specific cell types that might predict outcomes. In this blog, read more about their quest to find drug targets to prevent or postpone treatment resistance in patients with CML.
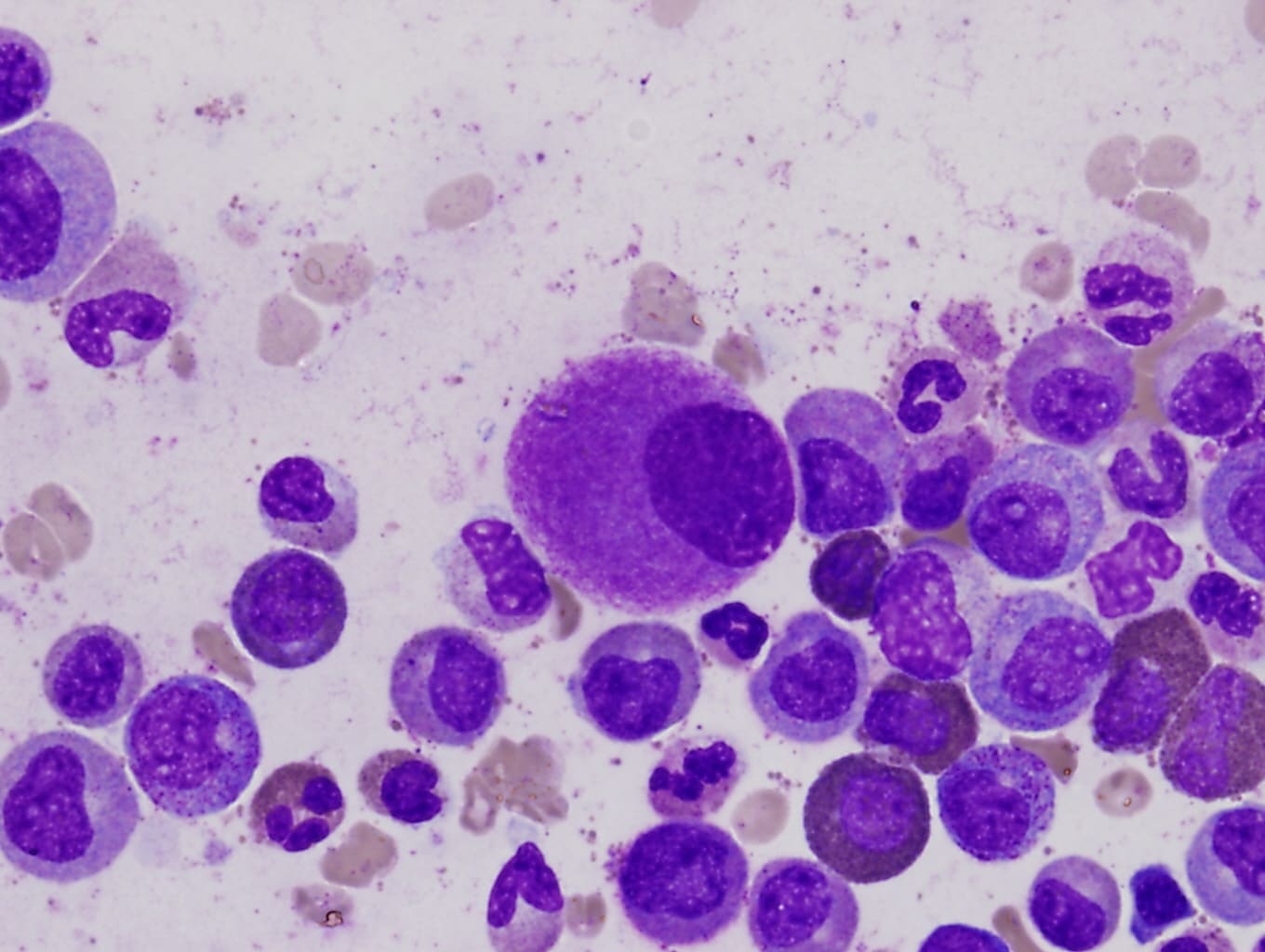
Chronic myeloid leukemia (CML) is a cancer that originates in the bone marrow (BM). Immature myeloid cells that reside in the marrow normally differentiate into red blood cells, platelets, and most types of white blood cells. However, in CML, a mutation in the BCR-ABL kinase gene turns the myeloid cells into CML cells, which start to escape the BM into blood and cause symptoms of the disease, including weakness, fatigue, and shortness of breath (1).
BCR-ABL tyrosine kinase inhibitors (TKIs) are effective but only for some patients—40% show a major molecular response (MMR) within 12 months, but 10 to 15% of patients will advance to blast crisis (BC), which is an end stage (2). CML is difficult to treat once it’s reached the BC phase, as available TKIs aren’t very effective, often leaving BM transplant as a patient’s only option. Uncovering what factors might contribute to primary TKI resistance—especially those that might exist before patients begin treatment—could reveal molecular biomarkers that predict TKI response.
In recent work led by Vaidehi Krishnan, PhD, at Duke-NUS Medical School in Singapore, scientists used single cell transcriptomic profiling of three groups of CML patients with increasing TKI resistance (3). They identified eight features in the pre-treatment BM samples that correlated with sensitivity or resistance to imatinib (a first-line TKI). By using machine learning methods, they characterized leukemic stem cell (LSC) and natural killer (NK) cell transcriptomic profiles that could be used to predict imatinib response with greater than 80% accuracy.
Single cell atlas characterizes the treatment response landscape
Dr. Krishnan took BM samples from CML patients divided into three groups with increasing TKI resistance (group one, MMR to imatinib; two, better response to second- or third-line TKIs; and three, resistance to all TKIs with progression to BC). The researchers employed Chromium Single Cell Gene Expression to create a single cell transcriptomic atlas, in which they described 32 cell populations (or cell types): 10 CD34+ hematopoietic stem and progenitor cell (HSPC) and 22 CD34- differentiated populations, including 8 myeloid, 7 B-cell, and 7 T/NK-cell populations.
Eight pre-treatment factors can predict TKI response
The team used machine learning to identify specific gene expression signatures in LSCs and NK cells at time of diagnosis that best predicted TKI response. In patients with MMR, there were two types of LSCs that predicted sensitivity to TKI: one was associated with erythroid progenitor expansion in vivo (or, premature red blood cells) while a second belonged to a subset of “hyperfunctional adaptive-like” NK cells (or, a specific type of tumor-killing NK cell). They saw that, in the patient groups with increasing resistance to TKI therapy, the proportions of these LSC cells changed; specifically, there were fewer LSCs with erythroid-biased fates and more with MYC- and IRF1-driven gene expression.
On the other end of the spectrum, in patients with BC, they found more inhibitory NKG2A+ NK cells. The authors suggest that, since the NK cells exist in either an activated state (in MMR patients) or an HSPC-tolerant state (in BC patients), these cells could be used as predictive biomarkers or to inform patient stratification when studying NK cell–based therapies.
A comprehensive and effective biomarker would likely include multiple pre-treatment factors, which they defined as erythroid-primed LSC, erythroid progenitor, myeloid progenitor, adaptive NK cell, MYC-primed LSC, patient-specific clonal expansions, KLRC1+ NK cell, and inflammation. Taking into account all these factors before treatment, and not just the abundance of a few specific cell types, will afford patients the best chance at tailored therapy, the authors believe.
Future focus: Biomarkers for TKI response in CML
Knowing if a patient with CML is prone to progress to BC will lead to more timely, life-saving treatments. The earlier a BM transplant is performed, the more effective it will be; and knowing a patient is at high risk of developing resistance to TKI therapy can mean earlier and more effective treatment. By combining single cell and AI, scientists are forging new ground in the development of biomarkers for response to CML therapy and, eventually, the identification of drug targets to improve or even altogether prevent treatment resistance and BC in CML.
References:
- https://www.cancer.org/cancer/types/chronic-myeloid-leukemia.html
- Braun TP, et al. Response and resistance to BCR-ABL1-targeted therapies. Cancer Cell 37: 530–542 (2020).
- Krishnan V, et al. A single-cell atlas identifies pretreatment features of primary imatinib resistance in chronic myeloid leukemia. Blood 141: 2738–2755 (2023).
