Allen Institute healthy human immune cell atlas scales to over 16 million single cells
*Impact at a glance: This study used single cell sequencing to look at 16 million cells from nearly 400 people and found age-related changes in specific immune cell types that may negatively impact immune function in older adults. These insights provide targets for developing drugs that keep the immune system strong throughout life.*
“The function of immune cells is always dictated by some element of time.” – Gong Q, et al (1).
Time seems to be an enemy to us all, even the cells that make up our bodies. Immune cells are a mysterious and incredibly important class of cells that protect us from pathogens, but normal aging processes can change their composition and function. These changes may hold the key to why certain diseases like arthritis generally appear with age or why the immune response weakens over time. And perhaps, if we define them, these patterns of change can be disrupted to improve human health in aging.
The search for a comprehensive understanding of how immune activity changes with age led a team of scientists from the Allen Institute for Immunology to dedicate years of research, hundreds of patient samples, and millions of single cells towards building a large-scale single cell atlas of healthy human immune cell composition. In the words of the authors, “This effort resulted in a high-resolution scRNA-seq resource comprising over 16 million peripheral immune cells from more than 300 healthy individuals aged 25 to 90 years” (1).
Keep reading to explore findings from their bioRxiv preprint about the T- and B-cell dynamics that could be driving immune dysregulation with age. And learn how Chromium Single Cell Gene Expression and Gene Expression Flex supported this project, including allowing assay modifications to scale the number of cells analyzed per microfluidic run and compatibility with fixed patient samples for flexible analysis of donor samples and efficient sample batching.
Why single cell resolution and massive scale is essential to establish patterns of immune change in aging
Whether it’s a matter of training an algorithm or discerning subtle changes in cellular and molecular composition between biological samples, pattern recognition requires data—a lot of it—and a level of resolution and quality that matches the complexity of the system being studied. In order to understand how immune cell composition and function change with age, researchers from the Allen Institute for Immunology needed single cell–resolution data from many diverse individuals across the age spectrum and enough cells per sample to properly represent the breadth of cell types in the peripheral immune system. This required a single cell technology platform with the flexibility to scale up analysis in unprecedented ways.
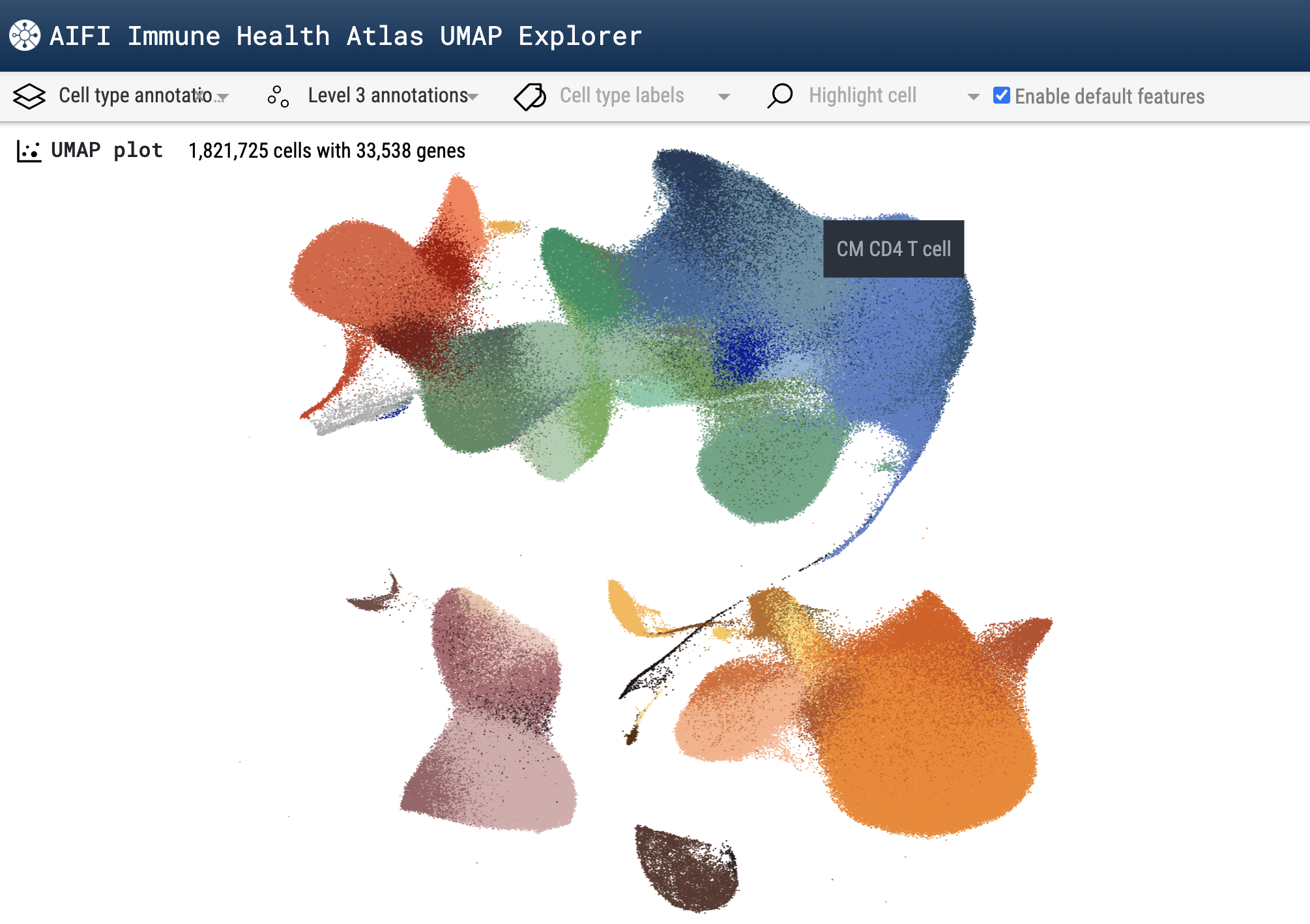
Using the Chromium Single Cell 3’ assay provided the resolution of individual cells and a platform with flexibility to enable cell hashing and overloading of up to 64,000 cells per well to maximize the scale achieved in each run. Sampling peripheral blood mononuclear cells (PBMCs) from a cohort of over 100 healthy individuals between 11 and 65 with this approach, the team was able to profile an average of 15,000 cells per donor. In total, this generated a dataset of 1.82 million PBMCs.
Importantly, because the Allen Institute researchers were able to generate high-quality data from a large number of cells per donor, they could resolve rarer, yet functionally important, peripheral immune cell subtypes. This included CD27- TBX21+ effector B cells, which are involved in the response to flu vaccination, and a recently characterized circulating KLRC2+ CD8-alpha alpha T-cell population, with qualities that suggest they are poised for rapid effector responses, but that may be lost globally with age (1,2).
But, in order to capture a complete picture of immune change with aging, the team determined they would need to do more than compare immune composition between donors at different ages. They would also need to incorporate analysis of longitudinal samples from the same individuals. To do this, they sampled PBMCs from a cohort of 49 young adults (25-35 years old) and 47 older adults (55-65 years old) over the course of two years, with all donors providing 8 to 10 blood draws (including several post-vaccine blood draws to enable comparison of age-related differences during vaccine-induced perturbation to homeostatic maintenance).
Across these longitudinal samples, the research team compiled an scRNA-seq dataset of over 13.7 million cells, from which they could derive meaningful insights about the patterns of cellular and molecular change that take place in healthy aging.
To further confirm the compositional and transcriptomic changes they observed in the immune cell data they’d accumulated from the 3’ assay, the team went even deeper, profiling immune cells from an additional cohort of 234 healthy adults that were 40 to 90+ years of age. However, these PBMCs were fixed, which provides the benefits of preserving cell states for downstream profiling on a flexible schedule and greater efficiency in sample batching. Therefore the research team chose to use the Chromium Single Cell Gene Expression Flex assay to conduct this round of single cell analysis. Flex uses a different assay chemistry to provide high-quality scRNA-seq data from fixed samples, including FFPE tissue, and can even be used for partially degraded samples that are inaccessible to other scRNA-seq approaches. These factors supported a high-throughput experimental workflow: the team was able to run batches of either 48 or 64 samples, and the chip configuration for the Flex assay allowed superloading of 400,000 cells per well. This produced a dataset of 3.2 million PBMCs.
T- and B-cell dynamics in human aging reveal possible mechanisms for age-related immune dysregulation
The immune system is not only involved in the onset of age-associated diseases, but it also influences how we respond to treatments for different diseases. Vaccines for the flu and SARS-CoV-2, or cell-based cancer therapies like CAR T cells, can have varying effectiveness depending on the composition and condition of the recipient’s peripheral immune system. Defining the condition of the healthy immune landscape over time is therefore of great urgency in designing more effective, age-specific treatments that can intercept the immune mechanisms at work in disease and accommodate for the immune changes that accompany aging.
Focusing on the longitudinal scRNA-seq dataset, which included over 13.7 million PBMCs, the Allen Institute research team sought to understand the differences in immune cell composition and transcriptional profiles of specific immune cell subsets over the course of aging. Their dataset included over 3 million T cells, 1.2 million B cells, 1.1 million NK cells, 2.4 million monocytes, 123,020 dendritic cells, and 10,431 hematopoietic precursors, providing a rich resource to interrogate detailed cell states, differentially expressed genes (DEGs), and functional relationships between these important immune cell types.
One takeaway from the team’s abundant data was that the relationships between T and B cells play a major role in modifying immune function in aging. The team found that, over time, T-cell subsets had the highest number of age-related DEGs, while many other immune cell subsets exhibited no significant age-related changes in their transcriptomes. Naive CD4 T cells had the most DEGs (n=331) but didn’t change significantly in frequency; naive CD8 T cells also had major transcriptional changes (n=182) and decreased in frequency with age (which is a hallmark of immune aging). Among other age-susceptible T-cell subsets, central memory and effector memory CD4 and CD8 T cells showed consistent transcriptional differences with age in the longitudinal cohort.
B cells also showed changing profiles with aging, specifically in the post-vaccination context. The longitudinal cohort included samples taken from donors after seasonal flu shots, but the team observed that core memory B-cell subsets had reduced expansion in older donors, meaning fewer cells involved in this important protective response to pathogens were activated as a result of vaccination, which could translate to a slower or weaker overall immune response. Additionally, CD27-effector B cells had lower expression of immunoglobulin G (IgG) genes—responsible for antibody production, typically as a secondary immune response to pathogens (3)—following vaccination in older donors, suggesting a decline in antibody class-switch responses with age. This is an important finding to better understand how age could affect vaccination efficacy.
Given these T- and B-cell dynamics, the team hypothesized that, like a cascade effect, changes in core memory CD4 T-cell helper functions with age may have downstream effects on B-cell subsets typically activated by this T-cell population. Leveraging a cell–cell communication inferring software called CellPhoneDB to investigate T- and B-cell receptor–ligand interactions, they discovered that core memory CD4 T cells from older donors had reduced predicted interactions with core memory B cells, specifically between CD40LG:CD40, a key complex for B-cell activation. This likely stemmed from a loss of the surface ligand CD40LG on T cells over time, which was a confirmed finding in single cell gene expression data from the follow-up cohort (marked by a decrease in expression of CD40LG in core memory CD4 T cells across the aging spectrum). Importantly, this result may point to targetable pathways that can be further explored to ensure a consistently robust memory B-cell response to pathogens with aging.
These findings represent just a small part of the Allen Institute for Immunology’s larger study, which you can explore in their preprint. Their pioneering efforts to combine single cell RNA-seq analysis with longitudinal sampling at scale have provided an unprecedented depth of cellular and molecular insights into the aging immune landscape and point us to new possibilities across biological fields. You can explore their datasets here. For a beautiful introduction to this study and what single cell data can look like, we also recommend you explore Nature’s Palette: A tale of science and art.
Our Chromium Single Cell platform is now powered by GEM-X technology. Learn more about our new solutions, including GEM-X Flex Gene Expression and GEM-X Universal 3’ and 5’ Gene Expression Multiplex.
References:
- Gong Q, et al. Longitudinal multi-omic immune profiling reveals age-related immune cell dynamics in healthy adults. bioRxiv (2024).
- Thomson Z, et al. Trimodal single-cell profiling reveals a novel pediatric CD8αα+ T cell subset and broad age-related molecular reprogramming across the T cell compartment. Nat Immunol 24: 1947–59 (2023). doi: 10.1038/s41590-023-01641-8
- Justiz Vaillant A, et al. Immunoglobulin. [Updated 2023 Aug 28]. In: StatPearls [Internet].
About the author:

Blog contributor: This article has been reviewed for scientific accuracy by Angela Churchill, PhD.

