Unlocking lung tumor heterogeneity: single cell analysis reveals a high-plasticity cell state
While there are numerous treatment options for lung cancer, it remains a notoriously difficult cancer to treat if not caught early since most lung tumors eventually become resistant to chemotherapy, a mainstay treatment. For Lung Cancer Awareness Month, we feature recent research that underscores the potential of single cell techniques to uncover drivers of tumor progression and treatment resistance. In this work, scientists discovered a new, highly plastic cell state that they believe plays a large role in tumors becoming resistant to chemotherapy. Read more to learn how single cell transcriptome profiling and chromatin accessibility mapping is allowing scientists to discern surprising insights into tumor evolution.
Lung cancer is the leading cause of cancer death for both men and women, comprising about 25% of all deaths from the disease. More people die of lung cancer than of colon, breast, and prostate cancers combined every year. There are two broad histological classifications of lung cancer, small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). NSCLC and its subtypes, adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, account for about 85% of lung cancers. Patients have a higher five-year survival rate if they are diagnosed earlier, before the cancer has spread outside the lung to either nearby structures or more distant parts of the body.
While there are many types of therapies to treat lung cancer based on stage and in some cases, genotype, chemotherapy is still standard treatment for both NSCLC and SCLC. However, some lung tumors are essentially resistant to chemotherapy, and in almost all cases, even those that respond at first will develop resistance to treatment—ultimately limiting the ability to effectively treat advanced lung cancers (1).
Cancer tumors of all types are known for being heterogeneous, which means they are composed of many different cell types and functional cell states. While it is believed that genetic mutations in tumor cells are the major driving force in tumor progression, how tumors evolve is not very well understood. Single cell techniques are allowing researchers to take a more in-depth look at tumor heterogeneity, evolution during cancer progression, and treatment responses. Understanding how tumors actually develop chemo-resistance will go a long way toward creating more effective therapies for advanced cancers.
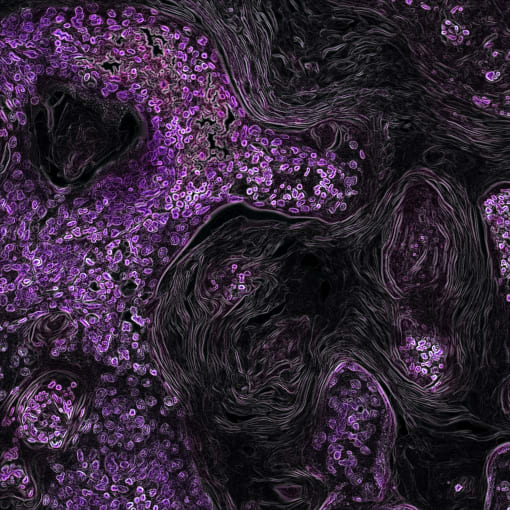
In a recent study, scientists led by Dr. Nemanja Despot Marjanovic at the Broad Institute of MIT and Harvard took advantage of single cell techniques to study lung adenocarcinoma (LUAD) in mouse models (2). Using single cell RNA-sequencing (scRNA-seq), the team profiled single cell transcriptomes of mice lung tumors at different stages of cancer progression, from pre-neoplastic hyperplasia to adenocarcinoma (they collected 3,891 single cell transcriptomes from 39 mice at eight distinct stages of LUAD evolution). They determined that cellular heterogeneity increased over time, that these increasingly diverse transcriptomes were reproducible, and that they were not caused by genetic diversity (specifically, copy number variation). Looking deeper, they discovered that most of the transcriptome populations had features of intestinal and/or gastric or embryonic liver epithelium—all endodermal tissues derived from the embryonic primordial gut. In essence, these cells no longer entirely resembled lung cells, pointing to the possibility that cells can become alternative types.
Of the different transcriptional populations that they revealed, one stood out: a highly mixed population of different cell types, ranging from trophoblast stem cells to chondroblasts and kidney tubular epithelium. They named this a “high-plasticity cell state” (HPCS), and cells in this state, they believe, can become many different kinds of cells. The HPCS serves as a transitional state that allows cells to assume new phenotypes and become chemo-resistant.
They then used single cell assay for transposase-accessible chromatin sequencing (scATAC-seq) to find that, at the signature genes in the HPCS, there was increased chromatin accessibility—and that this predicted tumors becoming metastatic. In other analyses, they concluded that mouse HPCS cells grew more and faster and had increased chemo-resistance than other non-HPCS tumor cells—and that they are distinct from both cancer stem cells and other stem cells. Importantly, combining scRNA-seq profile data and the Cancer Genome Atlas (TCGA) bulk RNA-seq data, they determined that this cell state also exists in human lung tumors and is associated with poor survival. Looking deeper, they discovered that this state could be used to predict poor outcomes across all tumor types in TCGA, suggesting that similar high-plasticity cell states may exist in other types of human tumors.
Pointing toward a paradigm shift in treating advanced tumors
This work positions the HPCS as a key driver of treatment resistance in lung cancer, pointing to a possible new type of drug target. Considering that most advanced lung cancers eventually become chemo-resistant, new drug targets are key to more effective therapies. Possibly, combining chemotherapy drugs with new drugs targeting this highly-plastic cell state may help better prevent resistance and tumors recurring after treatment. In addition, single cell techniques will help scientists further explore and determine the role of a high-plasticity cell state in other tumor types, giving us a richer understanding of tumor heterogeneity and a broader application of this new class of cancer drug target.
Explore our resources to learn how you can gain a multidimensional view of cancer and dissect the interactions between the tumor and immune environments.
References:
- ES Kim. Chemotherapy Resistance in Lung Cancer. Adv. Exp. Med. Biol. 893, 189–209 (2016).
- ND Marjanovic et al., Emergence of a High-Plasticity Cell State during Lung Cancer Evolution. Cancer Cell. 38 (2), 229–246.E13 (2020).
